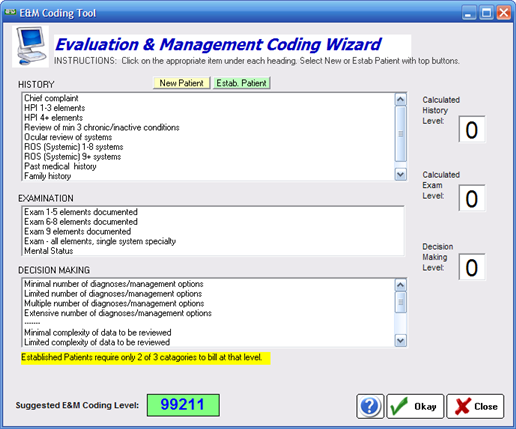
A simple tool to allow you to code the exam for Medicare E&M requirements. To use the tool, select New or Established patient. Then click on each of the items you have completed in each of the three categories (history, examination and decision making). As you select items the appropriate code will be calculated and displayed.
E&M Coding Guidelines
Proper coding encompasses three areas: History, Examination and Medical Decision Making
History
The History comprises four parts parts:
| • | Chief Complaint |
| • | History of the Present Illness (HPI) |
| • | Review of Systems (ROS) |
| • | Past History, Family History, and Social History (PFSH). |
Chief Complaint
The chief complaint is the primary reason for the patient's visit, which may be in the patient's words or the provider's summary.
History of the Present Illness
The HPI is composed of eight elements:
| • | Location |
| • | Duration |
| • | Severity |
| • | Quality |
| • | Timing |
| • | Context |
| • | Modifying Factors |
| • | Associated Signs and Symptoms |
The HPI is divided into Brief and Extended, Brief has one to three elements and Extensive has four or more elements described.
Review of Systems (ROS)
The systems are: Constitutional — Eyes, Ears, Nose, Mouth, Throat; Cardiovascular — Respiratory; Gastrointestinal; Genitourinary; Musculoskeletal; Integumentary (skin and/or breast); Neurological; Psychiatric; Endocrine; Hematologic/Lymphatic; and Allergic/Immunologic.
Personal, Family & Social History
For the PFSH, you must ask one question for each category in order for that category to be considered inventoried.
Examination
Each item identifies an element that the provider must perform if that element is to be counted toward the level of the examination. No substitutions are allowed — you cannot take elements from other single organ systems and count them as eye examination elements. A total of 14 elements are identified by a bullet. At the highest level, all 14 have to be performed.
| • | Test visual acuity (does not include determination of refractive error) |
| • | Gross visual field testing by confrontation |
| • | Test ocular motility including primary gaze alignment |
| • | Inspection of bulbar and palpebral conjunctivae |
| • | Examination of ocular adnexae including lids (eg, ptosis or lagophthalmos), lacrimal glands, lacrimal drainage, orbits and preauricular lymph nodes |
| • | Examination of pupils and irises including shape, direct and consensual reaction (afferent pupil), size (eg, anisocoria) and morphology |
| • | Slit lamp examination of the corneas including epithelium, stroma, endothelium, and tear film |
| • | Slit lamp examination of the anterior chambers including depth, cells, and flare |
| • | Slit lamp examination of the lenses including clarity, anterior and posterior capsule, cortex, and nucleus |
| • | Measurement of intraocular pressures (except in children and patients with trauma or infectious disease) |
| • | Ophthalmoscopic examination through dilated pupils (unless contraindicated) of optic discs including size, C/D ratio, appearance (eg, atrophy, cupping, tumor elevation) and nerve fiber layer |
| • | Posterior segments including retina and vessels (e.g. exudates and hemorrhages) |
| • | Brief assessment of mental status - orientation to time, place and person |
| • | Brief assessment of mental status - mood and affect (e.g. depression, anxiety, agitation) |
Medical Decision Making
The levels of E/M services recognize four types of medical decision making (straight-forward, low complexity, moderate complexity and high complexity). Medical decision making refers to the complexity of establishing a diagnosis and/or selecting a management option as measured by:
| • | the number of possible diagnoses and/or the number of management options that must be considered; |
| • | the amount and/or complexity of medical records, diagnostic tests, and/or other information that must be obtained, reviewed and analyzed; and |
| • | the risk of significant complications, morbidity and/or mortality, as well as co-morbidities, associated with the patient's presenting problem(s), the diagnostic procedure(s) and/or the possible management options. |
Medical Decision Making is the most difficult of the three key components in E/M coding to master. The grid below gives a rough idea of what constitutes Decision Making:
Number of diagnoses or management options |
Amount and/or complexity of data to be reviewed |
Risk of complications and/or morbidity or mortality |
Type of decision making |
Minimal |
Minimal or None |
Minimal |
Straightforward |
Limited |
Limited |
Low |
Low Complexity |
Multiple |
Moderate |
Moderate |
Moderate Complexity |
Extensive |
Extensive |
High |
High Complexity |
Audit Flags
Some of the common documentation problems (extracted from Optometric Management):
| ► | Confrontation visual fields not addressed; if not done — state the reason. |
| ► | Primary gaze alignment is not "versions full" — you must address the primary gaze measurement. |
| ► | No reason given when intraocular pressure (IOP) is not measured. |
| ► | Pupils not dilated, and the two elements (optic nerve and posterior segment) are still being counted toward the level of the exam — with no explanation as to why. It has to be a medical contraindication — not that it's "a sunny day." |
| ► | Neurological/Psychiatric elements missing. |
| ► | Dilating drops not listed in the chart. |
| ► | Failure to check off normals for each eye, particularly when there is a problem in the other eye. |
| ► | Failure to describe the abnormality. |
| ► | Failure to perform all 14 elements. |
| ► | You cannot count an extended ophthalmoscopy as the basic elements of optic disc and posterior segment and also as the separate diagnostic test, extended ophthalmoscopy. |
| ► | Note that the word "referral" does not appear in the document. You do not receive credit for referring a patient. |
| ► | When considering number of diagnosis or management options, this refers to the examiner and not the practice (what others have diagnosed). |
| ► | When coding encounters for established patients, be sure to use both number of diagnosis/management options and risk of complications. |
| ► | Requesting a consultation is not an activity that can be counted under Amount and Complexity of Data. |
| ► | Chief complaint and HPI technically are to be performed by you and you alone. You must perform or repeat any element that is counted in determining the level of the examination. |
| ► | Any element you are applying as an element performed when you select the level of the examination must be performed by the practitioner and not auxiliary personnel. |